Needed: More awareness of skin cancer in richly pigmented skin
A lack of knowledge among the public and physicians about the appearance of skin Ca in darker skin contributes to worse outcomes (1,500 words, 8 minutes)
Skin Spectrum Weekly is published with unrestricted support from Bausch Health Canada
Despite the lower incidence rate of skin cancer in darker skin types, the prognosis continues to be worse in this population than in White patients. That is typically due to later diagnosis, said Dr. Joël Claveau during a presentation at the 8th annual Skin Spectrum Summit.
He said these delays result from a lack of patient awareness and a need for’ need for more education.
“There is a big gap in the knowledge that dark-skinned people do get skin cancer,” said Dr. Claveau. “I do a lot of reports in the media about sun prevention, and every year I get the same question: “Do dark-skinned people have to protect their skin from the sun? Do they have to use sunscreen? It is something we have to repeat and repeat.”
He noted that a lack of skin cancer awareness among patients with darker skin might lead to alternate explanations for lesions. A dark spot on the foot might be explained as a stain, he said.
“[The mark] is not because the person walked on oil. That doesn’t stay for months,” Dr. Claveau said. “Patients often tell you stories like that.”
As a result, physicians must try to find the time to conduct a complete skin exam, he said. Acral melanoma is more common in Black skin, and the diagnosis can be easily missed if patients don’t remove their shoes and socks.
Part of the delay in diagnosing skin cancer in darker skin types may be due to a hesitation to biopsy lesions on the hands and feet, where some cancers appear more commonly in dark skin. However, Dr. Claveau said that advances in dermoscopy have made it easier to identify lesions that are likely benign without doing a biopsy.
“With the advance of dermoscopy, we can recognize patterns for benign nevi,” he said. “We have very good literature originally coming from Asia, Italy and from all over the world telling us which [lesions] are benign, which are malignant.”
If a nevus on a patient’s foot is benign on dermoscopy, “I do not need to biopsy and potentially give a callus and maybe [create] a problem with walking and jogging later on.”
Dr. Claveau provided several tips regarding patients with nevi in dark skin:
Ulcers on the lower limbs that do not heal for a long time should raise suspicion of squamous cell carcinoma.
Organ transplant patients with dark skin are as likely to develop squamous cell carcinoma as patients with White skin. Physicians should remember to screen these patients once or even twice a year for potential cancer.
Nevi are darker in darker skin. While dark-coloured nevi should not be assumed malignant, physicians should also not overlook lesions that are typically pink, such as pearly basal cell carcinoma, if they are darker.
Dark bands on the fingernails can be common and benign in Black children, so physicians should not be in a rush to biopsy, especially if all the nails on the hand or foot have these bands. A watch-and-see approach is better in these cases.
Bottom line: Late skin cancer diagnosis continues to be an issue for patients with dark skin types. Increased public awareness and physician training—especially in using the dermatoscope to quickly screen for benign or suspicious lesions—are needed to improve patient outcomes.
From the literature on skin cancer in skin of colour
Morphology of mycosis fungoides and Sézary syndrome in skin of colour
This paper's authors note that mycosis fungoides (MF) and Sézary syndrome (SS) commonly affect Black patients. However, medical educational resources mostly describe how these conditions appear in lighter skin.
The investigators reviewed clinical photographs of patients with Fitzpatrick skin types I-VI to determine the frequency of different morphologic features of MF or SS in patients with skin of colour vs. patients without skin of colour.
Combination of 1,550 nm non-ablative fractional resurfacing and laser hair removal for treatment of Becker's nevi in skin types III-VI
The investigators performed a retrospective review of patients treated between 2016 and 2021. Clinical photographs were graded by three independent physicians using a 5-point visual analog scale.
In this study, 12 patients with Fitzpatrick skin types III to VI and Becker’s nevus on the face, trunk, or extremities were treated with a combination of 1,550 nm non-ablative fractional resurfacing. The patients received an average of 5.3 treatments at one- to four-month intervals. Ten patients had laser hair removal on the same day as their resurfacing treatments.
The researchers followed the patients from six to 40 weeks (mean 10.5 weeks) after treatment. Among the 12 patients, the mean cosmetic improvement in hyperpigmentation and hypertrichosis from Becker’s nevi was 51%-75%. No long-term adverse events were encountered with or without laser hair removal.
Risk of cutaneous carcinogenesis with phototherapy in Indian subpopulation: A 10-year analysis and a review of literature
The authors of this study note that while U.S. studies have shown that PUVA phototherapy may have carcinogenic potential, studies done in Asian and Arabian-African populations have not yielded similar results.
They assessed the cancer-related safety of bath PUVA and narrowband UVB (NBUVB) phototherapy in an Indian population with Fitzpatrick skin types IV and V.
The study enrolled 1,300 patients who received phototherapy between Jan. 2006 and Oct. 2016. Of those, 929 patients had received PUVA, and 371 patients had received NBUVB for various dermatologic indications. The average follow-up period for PUVA was three years and 6.5 years for NBUVB.
Researchers found that the maximum cumulative dose of UVA and UVB that could be safely administered in these patients without causing cutaneous complications was 2,085 J/cm2 and 1,985 mJ/cm2, respectively.
None of the patients developed any features of cutaneous malignancy during their follow-up. The authors conclude the risk of developing cutaneous malignancy is negligible in this subset of patients.
UV exposure and the risk of keratinocyte carcinoma in skin of colour: A systematic review
This study was conducted to assess and synthesize the published data on the association between UV exposure and the risk of keratinocyte carcinoma (KC) in individuals with skin of colour.
Researchers searched the PubMed, Cochrane and Web of Science databases for relevant papers published from the launch of each database to Jan. 2022. For this review, the investigators included studies that examined UV exposure as a risk factor for KC in individuals with skin of colour. They used the UV index, irradiance, latitude, history of phototherapy, history of sunburn, or occupational exposure as measures of exposure to UV radiation.
From a total of 72,716 reports that appeared in the initial search, 12 articles with clinical data spanning the years 1990 to 2019 met inclusion criteria. These papers represented 32,970 KCs in individuals with skin of colour.
Among the relevant articles, eight studies found no association between UV exposure and KC, while four showed a positive association. Study types included one ecological analysis, nine cohort studies, and two case-control studies. The quality of the studies was rated from moderate to low (2b to 4).
Overall, the review authors conclude there is only moderate to low-quality evidence for an association of UV exposure with KC. They write that studies found no association among patients receiving phototherapy. Studies assessing non-phototherapy-related UV exposure, such as geographic location or occupation, found small positive associations in primarily East Asian individuals. There were no studies performed in the U.S., no studies among Black individuals, and only one among a Hispanic population. The authors write that more research is needed to assess whether these associations exist across populations of patients with darker skin types.
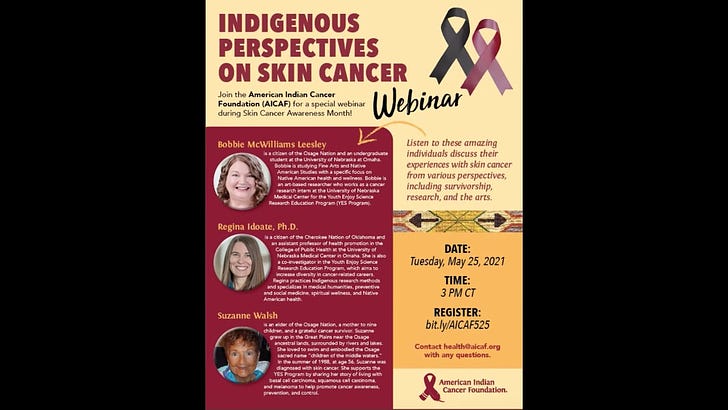
VIDEO: Indigenous perspectives on skin cancer
At the intersection of skin and society
An animated poetry anthology titled “Dreams in Vantablack,” featuring the work of 12 Black youth, premiered on CBC Gem on Sept. 29, 2022.
The anthology series is based on the writings of 12 Black youth poets from across Ontario between the ages of nine and 20 years, according to The Toronto Star.
According to the news article, issues explored in the episodes include mental health, identity, bullying, and racism.
Keteku said that the animators working with the poets understood the source material’s beats, nuances, and language because they were creators of colour themselves.
This week
October is Black History Month in the U.K.
October is Global Diversity Awareness Month
Oct. 3 is National Child Health Day in the U.S.
Something to think about in the week ahead…
In two weeks
On Oct. 17, Skin Spectrum Weekly will cover a talk by Toronto’s Dr. Renée Beach on the morphological differences in how atopic dermatitis presents in different skin types. The presentation was given at the 8th annual Skin Spectrum Summit in Sept. 2022.
Later this month
Drs. Perla Lansang and Neil H. Shear are pleased to announce the 2022 edition of the Great Lakes Immunodermatology Exchange (GLIDE 4.0) coming up on Oct. 21 and 22, 2022. The meeting will focus on catching up on the rapidly advancing field of immunotherapy. Topics include new concepts and therapeutics in real-world practice. For more information or to register, visit GLIDECanada.ca
If you like Skin Spectrum Weekly, why not check out our other publications, podcasts and portal?
Established in 1995, The Chronicle of Skin & Allergy is a scientific newspaper providing news and information on practical therapeutics and clinical progress in dermatologic medicine. The latest issue features:
Dr. Derek K. Chu (Hamilton, Ont.) discusses the findings of a review of the evidence for bleach baths as a treatment for atopic dermatitis
A review of recent advances in the understanding and treatment of hidradenitis suppurativa, featuring interviews with Dr. Raed Alhusayen (Toronto), Dr. Alia Bosworth (Halifax), Dr. Susan Poelman (Calgary) and Dr. Lauren Lam (Calgary)
Plus regular features, including the popular column “Vender on Psoriasis” by Hamilton, Ont. dermatologist Dr. Ron Vender.
To apply for a complimentary* subscription or to receive a sample copy, please email health@chronicle.org with your contact information.
The Women in Dermatology e-newsletter updates new findings concerning dermatologic issues that affect women and the female dermatologists who care for them. Read the current issue here.
Season three of the Vender on Psoriasis Podcast featuring Canadian dermatologist Dr. Ronald B. Vender is coming soon. Watch this space for updates.
And if you’re looking for a web destination for all things derm, please visit derm.city, “Where Dermatology Lives.” Please like it, rate it, and share it with your colleagues.